Global Impact
Vanderbilt University researchers are scouring the world to reveal the secrets of cancer.
November 21, 2013 | Bill Snyder

Photo by Daniel Dubois
From the bustling streets of Shanghai and Lusaka, to the dairy and potato farms of Túquerres, on Colombia’s high Andean plateau, Vanderbilt University researchers are scouring the world to reveal the secrets of cancer.
Aided by the latest genomic technologies as well as tried-and-true, door-to-hut epidemiology, these modern-day explorers are mapping out a previously unimagined topography of growth gone bad. What drives them is the conviction that what they find will benefit people everywhere.
“Today in parts of Africa, Asia and Latin America, treatable cancer is a death sentence,” noted Sten Vermund, M.D., Ph.D., director of the Vanderbilt Institute for Global Health.
“Not all countries have the resources we have to do something to improve health,” added Wei Zheng, M.D., Ph.D., MPH, Ingram Professor of Cancer Research and director of the Vanderbilt Epidemiology Center. “We can do that … and what we discover in another country can also help us improve our health in this country.”
Vermund, Zheng and their colleagues have joined forces with the Vanderbilt-Ingram Cancer Center (VICC) to develop a new Global Health Initiative. Its mission includes:
- Continuing and expanding existing international research collaborations that advance our understanding of cancer epidemiology, prevention and control;
- Building research capacity and training researchers in low-resource countries to help relieve disproportionately high burdens of cancer, some forms of which are entirely preventable;
- Attracting and training new investigators in global cancer research; and
- Helping Vanderbilt and VICC become leaders in global cancer research, treatment and prevention.
The China connection
Vanderbilt-led studies of breast, colorectal and other cancers based in Shanghai, China, have shown how the interaction of genetics, environment and diet contribute to these diseases and are offering novel ideas for treating and preventing them.
These are the Shanghai Women’s and Men’s Health Studies, established and led respectively by Zheng, who also is chief of the Division of Epidemiology, and Xiao-Ou Shu, M.D., Ph.D., MPH, professor of Medicine. Both are Ingram Professors of Cancer Research.
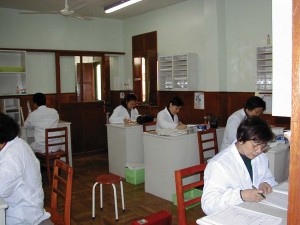
Research team members code questionnaires and check survey quality in the Shanghai Women’s and Men’s Health Studies.
With 75,000 research subjects in the Women’s Health Study, and 61,000 in the Men’s, and with major support from the National Institutes of Health (NIH), the cohorts are among the largest in the world.
They have laid the groundwork for other studies in China, notably the Shanghai Breast and Endometrial Cancer Studies, and established the Asian Breast and Colorectal Cancer Consortia, which include researchers from several Asian countries and the United States.
By pooling medical information from more than 80,000 people participating in the breast and colorectal cancer consortia, Vanderbilt scientists and colleagues around the globe have been able to pluck several cancer-associated “needles” from the genomic “haystack.”
In other words, they have identified more than 20 variations in the DNA readouts or “genomes” of individuals that are associated with increased risk for breast and colorectal cancers. These variations are called single nucleotide polymorphisms, or SNPs.
In collaboration with scientists around the world, Vanderbilt investigators have helped to identify close to 100 genetic variations for cancers of the lung, ovary, prostate, pancreas, liver and multiple other sites.
A major technique is the GWAS—genome-wide association study—in which the DNA of a large number of research subjects is “genotyped,” or scanned, to look for cancer-associated SNPs.
By comparing differences in genetic inheritance between different populations, the researchers can “zone in” on genetic variations that may increase the risk of cancer, the probability of relapse, or affect one’s response to anti-cancer drugs.
The variations and where they’re located on the genome are revealing new insights about how cancers develop and are suggesting potential targets for new, more effective drugs to treat or even prevent cancer from occurring in the first place, Zheng said.
But genes alone don’t explain the cancer story. There is increasing evidence that the interaction of genetic and environmental factors, including diet, can set the stage for disease.
Shu and her colleagues, for example, have found that high consumption of soy foods by Chinese women is associated with a reduced risk of breast cancer. Soy intake also was related to reduced recurrence and mortality among breast cancer survivors.
Soy contains estrogen-like compounds called isoflavones as well as other chemicals that may have anti-cancer effects.
This kind of research would be difficult to conduct in the United States, Shu pointed out, because soy in this country is processed in a way that may dilute or eliminate some of its potentially helpful compounds, or mixed as a powder in other foods.
In addition, soy consumers in the United States tend to be health-conscious individuals. It’s harder to isolate the impact of soy-containing foods in American women who watch their weight and exercise regularly, lifestyle choices that also can reduce cancer risk.
At least when it comes to confirming the role of soy in breast cancer, these studies must be done in countries like China, Shu said.
A huge imperative
Every year, a half million women around the world are diagnosed with cervical cancer. A quarter million die from the disease, which is entirely preventable, simply because they lack access to basic and low-cost prevention, diagnosis and treatment services.
When cervical cancer kills women in the prime of their lives, it devastates families, leaves orphans behind and can destabilize entire communities. “From a humanitarian point of view, addressing this issue is a huge imperative,” said Vikrant “Vik” Sahasrabuddhe, MBBS, MPH, DrPH, research assistant professor of Medicine who currently is detailed to the Division of Cancer Epidemiology and Genetics at the National Cancer Institute (NCI).
For nearly a decade, Vermund, Sahasrabuddhe and their colleagues have worked with health officials and researchers in Lusaka, Zambia’s capital city, to reverse that trajectory. They have trained nurses to use a simple technique, visual inspection with acetic acid or VIA, to detect cervical lesions.
![africaVIA training[1]](https://momentum.vicc.org/wp-content/uploads/africaVIA-training1-300x216.jpg)
Trainees in Zambia learn to use table vinegar to detect precancerous lesions in an effort to prevent cervical cancer.
The screening program began with women infected with HIV who are at higher risk of developing cervical cancer. In the past seven years, more than 120,000 women have been screened.
Sahasrabuddhe and colleagues have published program evaluation research that has shown that for every 46 HIV-positive women screened, one death from cervical cancer is prevented. “That’s a very low cost-to-benefit ratio,” he said. “Using these simplistic and low-cost technologies, we can save lives.”
The cervical cancer screening program infrastructure was integrated within the successful program for getting services to AIDS patients funded in 2004 by the President’s Emergency Plan for AIDS Relief (PEPFAR), said Vermund, Amos Christie Professor of Global Health.
Supported by the NIH Fogarty International Center, the Cervical Cancer Prevention Program is a partnership of the Centre for Infectious Disease Research in Zambia (co-founded by Vermund in 2000), the Zambian Ministry of Health and the University Teaching Hospital in Lusaka.
Now called the African Centre of Excellence for Women’s Cancer Control, it is a major project of the Pink Ribbon Red Ribbon campaign, which includes the George W. Bush Institute, PEPFAR, Susan G. Komen Foundation, Bill & Melinda Gates Foundation, Joint United Nations Programme on HIV/AIDS and major corporate sponsors.
The program has been tested in several other countries, and has been launched on a national scale in Mozambique, Vermund said.
Cancer’s “Bermuda triangle”
Next to lung cancer, gastric cancer is the second leading cause of cancer mortality in the world.
While the highest incidence has been reported in developing countries in Latin America and East Asia, the disease also is on the march in the United States, due to a confluence of factors that includes immigration, poverty, genetics and diet.
“I describe it as a Bermuda triangle of risk exposures, with dietary, environmental, and host and bacterial genetic factors,” said Douglas Morgan, M.D., MPH, associate professor of Medicine, who has studied gastric cancer in Central America over the past decade.
Morgan first noted high rates of the disease while providing medical care to Honduran survivors of Hurricane Mitch, following on his service as a Peace Corps volunteer there.
Most gastric cancer is associated with chronic infection by the bacterium Helicobacter pylori (H. pylori), which thrives in the stomachs of half the people on earth.
It would seem reasonable that killing the bug with antibiotics in high-risk populations might prevent gastric cancer. A Vanderbilt-led study reported this year in the Journal of the American Medical Association that antibiotic treatment cleared chronic infection in most—but not all—of people in seven Latin American communities.
But while many populations with high levels of H. pylori infection also have high rates of gastric cancer, that’s not true in Africa and India. Even in the same country, the risk of gastric cancer can vary wildly.
In Colombia, for example, the incidence of gastric cancer among the mestizos of Túquerres, elevation 10,000 feet, is 25 times higher than it is among the Afro-Colombians (Colombians of African ancestry) in the port city of Tumaco—a mere 130 miles away.
Pelayo Correa, M.D., and his colleagues have discovered that the strain of H. pylori that infects residents of Tumaco is much less carcinogenic than the strain found among the mestizos, those of mixed indigenous and European (16th century Spanish Conquistador) ancestry.

Douglas Morgan, M.D., MPH, visits with local children in Latin America, where gastric cancer rates are the highest in the world.
“When you mix European and Indian H. pylori genes, the European genes predominate,” said Correa, Anne Potter Wilson Professor of Medicine who has studied cancer in his native Colombia for half a century. “So, I say that even the bugs are Conquistadores!”
There are dietary and host gene differences as well, said one of Correa’s main collaborators, Richard Peek, M.D., Mina Cobb Wallace Professor of Immunology and director of the NIH-funded Vanderbilt Digestive Disease Research Center.
The mestizos are more likely to have low levels of iron in their blood, a consequence of high-altitude living. This relative deficiency in iron compared to residents of the coast “enhances the pathogenesis of the bacteria,” Peek said.
Correa, Peek, Morgan and their colleagues have found that mestizos in Central and South America also have prevalent genetic variations which increase expression of interleukin 1-beta, a pro-inflammatory cytokine associated with the risk of gastric cancer.
In addition, H. pylori can generate “reactive oxygen species” like nitric oxide and hydrogen peroxide that, through a process known as “oxidative stress,” can damage DNA and lead to gastric cancer—even after antibiotic treatment has killed the bug.
Correa is working with Keith Wilson, M.D., Thomas F. Frist Sr. Professor of Medicine, who is studying oxidative stress caused by organic compounds called polyamines during H. pylori infection. They will test whether difluoromethylornithine (DFMO), which blocks ornithine decarboxylase, the enzyme that synthesizes polyamines, can interrupt what he calls the inflammatory “cascade” to cancer.
“There are other cancers that arise from inflammation,” Peek noted. “What we learn from H. pylori-induced … cancer can be transferred over to those … malignancies.”
Back in the USA
Gastric cancer, an infectious disease that disproportionately affects minorities, is a growing challenge in this country, in part because of immigration patterns. “One quarter of the United States will be of Hispanic origin within two decades,” Morgan predicted.
Another population at risk is African-Americans, who have twice the death rate from stomach cancer compared to whites, according to the NCI.
In the rural South, their rates of H. pylori infection also are very high—”almost as high as they are in China and some areas of the Third World where 80 to 90 percent of the population is infected,” said William Blot, Ph.D., research professor of Medicine.
Blot is principal investigator of the NCI-supported Southern Community Cohort Study, a partnership of VICC, Meharry Medical College and the International Epidemiology Institute.
Established in 2001, the cohort is tracking the health of 86,000 people, two-thirds of whom are African-Americans. “So far we haven’t seen the elevation of stomach cancer that we would have predicted given the incidence of H. pylori,” Blot cautioned. “This is still an early story.
“We’re getting there,” he continued. “Probably in 10 years we’re going to be pretty close on the treatment end, where the genetic makeup of the individual will affect what therapy is offered.
“We’re trying to do something parallel from the prevention end, to see if we can identify what combination of genetic makeup and environmental exposure could put somebody at risk,” Blot added. Researchers then could “tailor” interventions to limit exposure in groups with the highest cancer risk.
“Many of the challenges in developing countries are mimicked by challenges we have in our own backyard,” added Vermund. “Providing continuous services for someone with a chronic disease like cancer is a challenge for us in rural areas in Tennessee … (or) Alaska or Puerto Rico.
Vermund concluded: “We’re hoping lessons can be learned from low-cost approaches to cancer care in developing countries … (that) may help us achieve economies without compromising quality of care.”
