Journal Watch
January 14, 2025
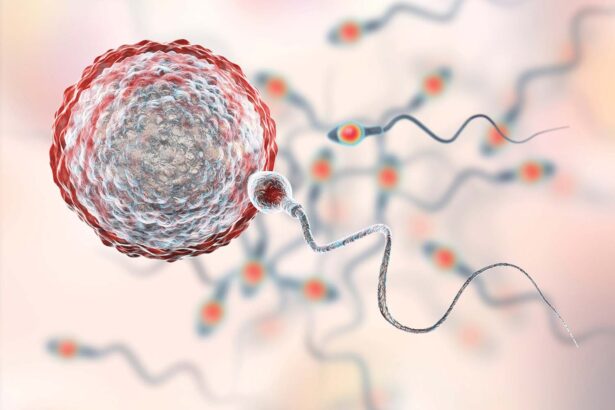
Only half of young cancer patients report discussing
fertility preservation
Only half of people with early-onset cancers reported discussing fertility preservation options prior to their oncology treatments, according to results of a cross-sectional study published Nov. 12, 2024, in JAMA Network Open. Young patients with thyroid, lung, ovarian and colorectal cancers reported the lowest prevalence of a fertility preservation discussion with a health care professional involved in their cancer care. Only 21.4% of patients with ovarian cancer reported a discussion about fertility preservation. The percentages reporting a discussion were 44.2% for patients with colorectal cancer, 21% for lung cancer, and 3.6% for thyroid cancer. The patient population represented 30 types of early-onset cancers.
In-clinic reconstruction of skin cancer defects costs less
Reconstruction of facial defects after skin cancer removal can occur in a traditional hospital-based operating room (OR) or an office clinic-based setting. Vanderbilt University Medical Center researchers compared cost-effectiveness for the reconstruction of facial skin cancer defects in the OR and clinic setting. The study, which was published Oct. 8, 2024, in Otolaryngology- Head and Neck Surgery, summarized the cost differences of head and neck reconstructive surgery for facial defects after skin cancer removal based on the procedural setting. Analyzing 1,206 patient cases from an insurance claim database, the researchers found that OR reconstruction cases had a higher median baseline cost of $2,308 compared to $987 for clinic procedures.
Study shows cancer vaccine blocks tumor progression at early lesion stage
A cancer vaccine that had little success in clinical trials for patients with advanced tumors could potentially have efficacy if administered earlier in the treatment cycle, according to a study from Vanderbilt researchers. The investigators demonstrated in a mouse model that the cancer vaccine can block tumor progression if administered when the lesions are at an early stage. Results of the study, which were published Oct. 3, 2024, in the Journal for ImmunoTherapy of Cancer, revealed that tumor-specific T cell populations are present in mice with early-stage lesions and can be therapeutically exploited by vaccination, but mice with advanced tumors do not retain these cells. The inquiry by the Vanderbilt researchers differed from most cancer vaccine studies, which have focused on patients with advanced tumors. The findings support further vaccine investigation to make long-term, progression-free survival a reality for more cancer patients, said the study’s senior author Mary Philip, MD, PhD, associate director of the Vanderbilt Institute for Infection, Immunology and Inflammation.
Protocol improves follow-up for women at high risk for breast cancer
A nurse-led initiative at the Vanderbilt Breast Center offers women at high risk for breast cancer greater opportunities for recommended follow-up screenings and genetic counseling. Before the new protocol was implemented, every patient underwent a Breast Cancer Risk Assessment Tool (BCRAT) evaluation, yet there was no established protocol for sharing the results. A team of six advanced practice providers devised a system using Epic software. Each week, they searched electronic health records to identify patients who had BCRAT scores with a lifetime risk of breast cancer greater than 20%. The scores were sent through a secure electronic message to the patients’ referring physicians notifying them of the option for an additional referral to the Vanderbilt Breast Center high-risk clinic. Nurses also contacted patients directly to offer high-risk consultations. Results of the intervention, which were published in the August 2024 issue of the Clinical Journal of Oncology Nursing, showed that the protocol resulted in increases in breast MRIs, genetic counseling and genetic testing. The study’s lead author is Ashley Johnson, DNP, APRN.
Epigenetic change to DNA associated with cancer risk
A research team co-led by investigators at Vanderbilt University Medical Center and the University of Virginia has identified associations between DNA methylation and cancer risk. DNA methylation is an epigenetic change — the addition of “methyl groups” to DNA — that can affect gene expression without changing the DNA sequence. Most DNA methylation occurs on CpG sites in the genome. The new study, published in the journal Nature Communications, identifies 4,248 CpG sites associated with the risk of seven different types of cancer: breast, colorectal, renal cell, lung, ovarian, prostate and testicular germ cell cancers.
No Comments »
No comments yet.
