Double Duty
Robotic technology makes simultaneous surgeries better for patients
August 6, 2024
Eighty-year-old Lois Taylor is getting a big kick out of telling everyone she knows that she’s a celebrity.
And she’s not wrong. Lois is the first person at Vanderbilt University Medical Center (VUMC) to undergo a fully robot-assisted, minimally invasive colon and liver resection to remove cancer performed by two surgeons under a single anesthesia.
The Russellville, Kentucky, resident came to VUMC after a routine colonoscopy in her hometown revealed a 3-centimeter lesion. She was referred to a surgeon and was shocked to learn the diagnosis: stage 4 colon cancer. Imaging revealed that her cancer had metastasized to her liver.
Overwhelmed, Lois listened to two proposals to treat the cancer from clinicians at other medical facilities. Both involved open surgeries, meaning large, open incisions to remove cancerous tissue. She was also told she wouldn’t likely be scheduled for surgery for a month or longer.
Her daughter, Geneva Taylor, has always marveled at her mom’s unflagging vitality and positivity. But she wasn’t so sure she could survive one or two major, open surgeries at her age, especially knowing there would be an extended period of postsurgery recovery and rehabilitation, likely followed by chemotherapy.
Geneva, who is Lois’ only child, is determined that one day her mom will hold her first grandchild, and both women were not at all convinced they heard the best option to make that possible.
“I called Vanderbilt and was connected to a patient advocate who, after they taught me how to share her records, bumped Mom’s appointment up to the very next week,” Geneva said. “That was amazing because when you hear that your mom has stage 4 cancer, you don’t want to wait a month or six weeks just to establish new patient care.”
The pair met with medical oncologist Rajiv Agarwal, MD, assistant professor of Medicine, Hematology and Oncology at Vanderbilt-Ingram Cancer Center. The mother and daughter quickly noticed a difference in how they were involved in decision-making during the consultation. Agarwal turned his computer screen around so they could follow along as he pointed out areas of concern on the scans of Lois’ colon and liver. He answered every question and put them both at ease.

Agarwal recommended an immediate consultation with his surgical colleague Kamran Idrees, MD, MSCI, MMHC, Ingram Associate Professor of Cancer Research, chief of the Division of Surgical Oncology and Endocrine Surgery, and director of Pancreatic and Gastrointestinal Surgical Oncology. Idrees has a global reputation as a leader in innovative surgical approaches to pancreatic and gastrointestinal cancers and is highly skilled in robot-assisted procedures.
“Ten years ago, we likely would have done at least one of these surgeries open or both of them open,” Idrees said. “We had a frank discussion with Lois and her daughter, Geneva, about the pros and cons of doing this procedure. The simultaneous presentation of liver metastases with a stage 4 presentation of colorectal cancer is not common, but we felt like she had a good functional status. We felt that she could tolerate both surgeries. And we know for a fact, that when we do robotic surgeries, we can do the same oncological or cancer operation that we need to do, and the recovery is faster.
“The liver is a completely sterile organ, so the risk of any infectious complication is really low. The colon is the polar opposite, full of bacteria. When the goal is to combine the two procedures, then the risk of infection goes up slightly. In carefully selected patients we can do the resections simultaneously,” Idrees said.
“Dr. Idrees involved Mom in the decision-making,” Geneva said. “He showed us the lesions on her liver and explained the difference between open surgery or a robotic surgery. After weighing our options and knowing Mom is 80, we knew we didn’t want her to have to recover from being open from basically sternum to pelvis. We decided we really wanted to do a robotic surgery.”
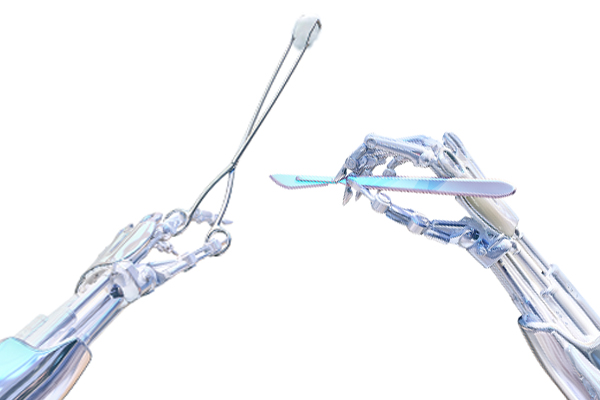
In open surgery, a large incision is made in the abdomen or pelvis, and the procedure is performed by a surgeon’s hands. In robot-assisted surgery, a surgeon manipulates a robot’s surgical tools through much smaller incisions while guided visually by a high-definition image captured by a three-dimensional camera on the tip of one of the robotic arms. Additional imaging such as CT or MRI scans can also be referenced for guidance during robot-assisted procedures.

The magnified view, as well as the dexterous, slender robotic arms allow the surgeon to clearly see and access areas that can often be difficult with traditional surgical techniques. Robot-assisted surgery typically results in less postoperative pain and fewer complications, as well as fewer days in the hospital and a quicker recovery time. This means if chemotherapy is required after cancer is surgically removed patients can begin this next stage of treatment sooner.
“Some might make the argument that for an 80-year-old patient combining two big surgeries does not make sense,” Idrees said. “On the other hand, putting someone this age through two different anesthetics and two surgeries at two different points in time may not be wise. You have to use clinical judgement in conjunction with the anesthesia team and all the involved parties. We felt like we could do it; we knew it was technically feasible; and we felt it would benefit this patient.”
Lois said she was never nervous about the procedures.
“I knew I had to have it done,” she said. “So, I said, ‘Get it out of here!’”
Idrees explained that he was one-half of the surgical equation, as he would be addressing only the cancer in Lois’ liver in the operating room. He knew just who to call for the colon resection — his colleague and expert in robot-assisted surgeries, Aimal Khan, MD, FACS assistant professor of Surgery.
Idrees and Khan reviewed Lois’ imaging together and spoke several times before her surgeries. Both men were confident they could perform a microscopically margin-negative resection for each organ, meaning leaving no trace of cancer behind in the colon and liver.
“I called the OR scheduler, Dora Snider, who’s incredible,” Khan said. “I told her we need to do this now, and we need to find time on a robot. You can’t just walk in, and a robot is waiting for you. Dora found us the room and the robot. We cleared our schedules, and we were operating within a week.”
Although they each had a game plan for their own surgery going in, the surgeons met in the operating room before the procedures began to marry the plans together and set up the robot, so both parts of the operation could be performed using the same incisions. The goal was to be as minimally invasive for their patient as possible, despite performing two significant procedures.
The surgeons marked where the incisions would best be placed for the access they needed, then they made small compromises, so only one set of incisions would be used to easily and safely achieve both resections.
Then Idrees began his surgery. A liver resection, or hepatectomy, is considered a technically difficult surgery, whether a surgeon is assisted by a robot or not. One reason is because the liver is laced with a network of small and large blood vessels, which can lead to substantial bleeding. The procedure is best performed by a highly experienced surgeon, such as Idrees, who can carefully navigate these vessels to remove only the cancerous tissue, leaving a clear margin.
During the surgery, Lois had enough blood loss that she required the transfusion of blood products. The surgeons and anesthesiology team watched her vital signs closely and paused to confer on whether it was wise to continue with the colon resection. Lois’ safety was always first in mind.
After a short break, she had stabilized, and Khan was able to begin the colon resection. An important factor for patients undergoing colorectal cancer surgery is the potential need for a colostomy. “Our anesthesia colleagues did an excellent job of stabilizing her in the middle of surgery, so I was able to remove the cancer and connect her colon back together, avoiding a colostomy,” Khan said.
Lois was up and walking unassisted within 24 hours of surgery. After she was discharged from the hospital, she went back home to Russellville, Kentucky, to continue what she calls an easy recovery. Geneva laughs when sharing that she would remind her mom to take her postsurgical medication, gabapentin, and Tylenol, for pain. Lois would often take just one Tylenol because she felt she didn’t need the prescription medication.
“I never got really sore after surgery,” she said. “Just a tiny bit, and it never bothered me once I got home. I got a little bit sick from the anesthesia, but I always do. That was it.”

Lois is finishing a 12-week course of chemotherapy overseen by Agarwal for “insurance” against a recurrence of the colon cancer, but she said it’s been much easier than she anticipated. She’s back to baking her famous rum cakes (she even treated Agarwal and his staff to one) and whipping up Southern-style meals for her family.
“I’m doing great,” she said. “I get tired more easily, but I haven’t been sick whatsoever. I’ve never taken any medicine for nausea. I’m gaining some weight, too. Everybody at Vanderbilt did such a great job taking care of me, and I’m so thankful for them.”
Khan and Idrees are hopeful that this success with synchronous robot-assisted colon and liver resections will lead to more such procedures at the Medical Center when the right patients are identified.
“It’s one of those things that when you do it, people then start realizing that we have the ability and the tools,” Khan said. “Not every patient will be a candidate for this, but for the patients that are, the benefits are going to be tremendous. And it may mean the difference between recovering from the surgery and maybe never recovering from it.”
For Idrees and Khan, the logic behind combining the two surgeries in one operating room, assisted by one robot, was never about achieving a first at the Medical Center, but rather about doing the best procedure to benefit the patient most with the highest likelihood of a good postsurgical outcome.
“The way I see it as a division chief, if we were going to move forward, the goal is always the best possible patient outcome, not personal accolades,” Idrees said. “Lois’ overall care highlights the strength of Vanderbilt-Ingram Cancer Center in regards to comprehensive multidisciplinary care, with multiple specialties including medical oncology, surgery and anesthesia under one roof, for cancer patients.”
“These are two major surgeries,” Khan said. “You must have the perfect team to do this. I would love to think that this success was the result of Dr. Idrees and my technical prowess, but it wasn’t. It was the OR staff, anesthesia and the nurses who help us with the robot. It was having the right technology. It was being here at VUMC where we have one of the best anesthesia teams in the country who can step in if a patient begins having issues. It was a team effort every step of the way.”
