20 Years
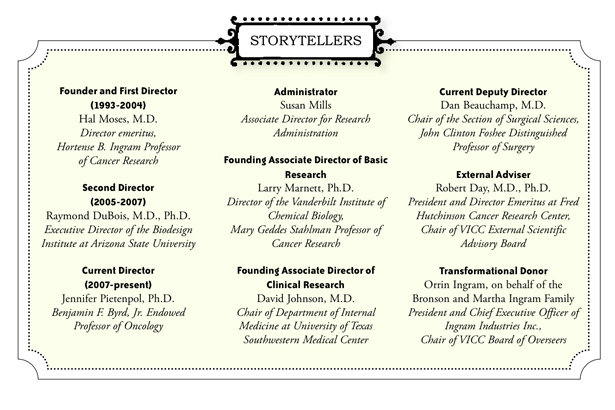
The major players recount VICC’s history in their own words
June 27, 2013

Over its 20 years, Vanderbilt-Ingram Cancer Center has grown and multiplied and grown some more, spreading into all parts of the University. It introduced new programs and resources, involving more and more scientists and clinicians and cultivating the highest level patient care, research and education. So much has changed in 20 years—mapping the human genome, understanding cancer pathways at the molecular level, discovering better drugs, and entering the digital age. But so much has stayed the same. The focus was initially—and is still today—to bring the best people together to make the biggest impact on cancer.
This is the story of a cancer center.
THE BEGINNING
By the 1980s, Vanderbilt University Medical Center had been offering cancer care for decades and basic research was strong, including Stanley Cohen’s Nobel-prize-winning work in epidermal growth factor. The A.B. Hancock Jr. Memorial Laboratory for Cancer Research and the Henry-Joyce Cancer Clinic were two building blocks Medical Center leadership believed a cancer center could be formed around that would be of the caliber for National Cancer Institute designation.
Marnett: We wouldn’t have been able to get a cancer center here no matter how good we were if there wasn’t a really strong base of research and clinical activity. The goal was taking what was here and making it a lot better. You want to float everybody’s boat.
Johnson: I think around 1983 they actually did make an application to the NCI [National Cancer Institute], but unfortunately it wasn’t successful. I think the feeling at the time, and I don’t know all the details, was that the committee felt highly of the institution and the research going on but thought the institution wasn’t ready to do this.
Moses: We didn’t have the grants. We didn’t have the investigators here, and we didn’t have the investments to recruit the faculty or build up the shared resources. The Medical Center was very poor in those days.
Marnett: They were sufficiently scarred from the process that nobody wanted to talk about it.
Johnson: In that next decade, the medical oncology program was stagnant. It would grow a little and retreat a little and grow a little and retreat a little.
-

1. An artist’s rendering of Medical Research Building II, when it opened in 1995. After a 54,000-square-foot expansion in 2001, it was rededicated the Frances Williams Preston Building. 2. Breaking ground on the Vanderbilt Cancer Center in 1993 were from left, Roscoe (Ike) Robinson, M.D., Hal Moses, M.D., Waddell Hancock, Frances Williams Preston, E. Bronson Ingram, Edward Nelson, Peggy Joyce and B.F. Byrd Jr., M.D. 3. Members of the VICC Board of Overseers, including Frances Williams Preston, third from right, see a lab demonstration in 1997.
Moses: For a long time Ike Robinson [then vice chancellor for Health Affairs] had wanted to get an NCI-designated cancer center at Vanderbilt, so I was on a search committee beginning somewhere around 1990 to bring somebody from the outside to direct the effort.
Johnson: I had made the decision to leave for another university because I felt Vanderbilt wasn’t serious about forming the kind of cancer center I wanted. We had had a long, protracted search for a cancer center director, and it just felt like we were wandering in the woods. It was never going to happen.
Marnett: It was obvious as we were bringing candidates in, that they weren’t as good as Hal Moses.
Moses: So just before Christmas 1992 Ike called me into his office and asked me to be the director.
Marnett: Hal came to me and asked me to consider being associate director for research. He went to David Johnson and asked him to be associate director for clinical science.
Johnson: I remember it vividly. Earlier that day I had verbally accepted a position at another institution. It was a Friday afternoon and Hal told me he decided to be the director and wondered if I would help. That wasn’t a hard decision to make. I was like a kid in a candy store given free rein.
Pietenpol: A remarkable clinician and investigator—David Johnson. An exceptional scientist with a lot of savvy in running programs—Larry Marnett. And then Hal, with his amazing breadth of talents, as director. I call them the three wise men.
Mills: It was very exciting because there weren’t a lot of brand new things starting up, especially something as broad and all-encompassing as the cancer center being described. Almost sight unseen they asked if I would be interested. I had not met Dr. Moses or anyone. It was a really big leap of faith but was so exciting.
I was literally given a handful of keys to space on what is now the 8th floor of the Robinson building. I opened up what was going to be the office area and it was nothing. There was just nothing there. Prowling around the space I found an old desk that was literally duct taped together. I found a chair that if I leaned back it would go over. So I had very good posture. If we got any phone calls when LifeFlight was landing we just had to stop. Because the space was so empty, everything reverberated. This was supposed to start off slowly, but once I got the desk and pulled a pencil out of my pocketbook, here we went. I never went back to the other job I had.
Marnett: Hal had an office that would hold his desk and one chair, no kidding. I think it used to be a closet.
Moses: The package for starting the Cancer Center was $5.6 million. It sounded like a lot of money then. $1 million of that was promised money from the T.J. Martell Foundation. That started our interaction with the music industry, which continues to flourish.
Pietenpol: Frances Preston [former president and chief executive of BMI] was very wise and recognized that we needed a cancer center in Music City. So she went to the Martell Foundation and asked for help to start this. Without funding from the T.J. Martell Foundation, the Joyce and Kleberg Foundations, and the Ayers, Hancock and Ingram families, we wouldn’t have had the strong start and infrastructure funding to continue. You think of a cancer center and the blocks that make the foundation—those are big, big ones. It put us in a position to be very competitive at the national level.
Marnett: The Hancock family had been very involved over the years supporting the Hancock Lab, and they’re very good friends with the Kleberg family. Some of the Kleberg family members, Helen Alexander and D.D. Matz, came down to visit. They are one of the few foundations that funds basic research. Because they’re involved in horse racing and breeding, they understand the importance of genetics. We took them first to the clinic to meet with David Johnson and he showed them around for about 45 minutes. He was extraordinarily gregarious and engaging. Low-key but lots of stories and sayings, funny and passionate. I’m thinking, “They’re so impressed with him. If he says they need money in the clinic that’s the way it’s going to go, not toward basic research as I hoped.” So he finishes the tour and says, “What you’ve seen is the best we can do right now. But the future of cancer treatment is what Larry is going to show you for the rest of the day.” That was completely unrehearsed. It was completely genuine. And it really impressed me. That was the case where a clinical director was spending his time targeting those donors for research. Perhaps years later it would help the clinic, but not right away. That set a tone for me really early that working together we could do a lot more.
In early 1994, Cancer Center leadership and administrators began seriously working on the Cancer Center Support Grant application to the National Cancer Institute. A successful application would bring an official designation from the NCI, funds to support infrastructure, and recognition on the national stage.
Marnett: NCI designation is important because it’s the imprimatur. It’s the stamp of approval. You can’t be a good cancer center without being an NCI-designated cancer center.
Marnett: We had an external advisory board and they were extremely helpful to us. They came in on Friday and reviewed what the research programs might look like. There were a couple of these programs that they just didn’t like. It was extremely painful because it was clear we could not go forward with some of those programs and it was going to be politically difficult for Hal.
Moses: I got a speeding ticket going home that night.
Johnson: Hal called an emergency meeting for Saturday. We looked at one another and said we have to make some really tough decisions.
Marnett: Hal and David looked like death that morning.
Moses: You’re reminding me of things that I had suppressed. It was really traumatic that first visit, but they told us what we had to hear and we corrected it.
Day: It was a matter of helping them see where the holes might be. I don’t think it was a disaster.
Johnson: It just illustrates that the things you do early are critical. You can make mistakes early with the best intentions. But using our external advisory board prevented us from making decisions that would have killed us at the time of the review. That’s the essence of leadership and a form of great courage. It was the right decision for the center as opposed to individual feelings. That was a defining moment and when we got over the hump frankly.
Moses: In a little over a year we had an application pulled together. We submitted it in September of 1994 and were site visited in January 1995.

1. Hal Moses, M.D., (left) and Orrin Ingram prepare to cut the cake at an employee celebration of the naming of Vanderbilt-Ingram Cancer Center in 1999. 2. Frances Williams Preston and Moses (right) talk with attendees at a Breast Cancer Survivors Celebration Tea in 1995.
Marnett: I can remember being in seminar the day before the site visit just trying to kill time because I had all this stuff in my head getting ready for it. Scared to death. Never done one of these before. I was just sitting there listening to this talk and almost passed out. I was so keyed up about what was going to happen the next day.
Moses: We got a priority rating of 191. That’s in the excellent range. It’s out of 500, 100 is best, 500 is worst. That was good enough to get funding, and we were the first new cancer center to receive NCI designation in a very long time.
Marnett: There hadn’t been a new NCI cancer center in 10 years.
Moses: I do admit that I was a little surprised we got it the first go-round.
Johnson: The biggest accomplishment was getting the NCI designation. Without that I’m not sure all else would have followed. Getting that recognition set the stage for all the greater things that occurred subsequently.
THE GROWTH
With NCI designation secured, the next goal was gaining Comprehensive status. In 1999 a transformational gift from the Ingram family gave the Cancer Center a new name and infused energy.
Marnett: At one point Hal was meeting with Orrin Ingram and Orrin asked him, “What would you do at Vanderbilt if money was no object?”
Ingram: On Dec. 1, 1994, my father [Bronson Ingram] was diagnosed with cancer, and he died on June 15, 1995. From the moment he was diagnosed we knew we were a lucky family with the means to go anywhere to get treatment, but he felt that Vanderbilt was as good as any place. But he died, so we knew it wasn’t good enough. I got frustrated that there wasn’t anything more we could do.
Moses: The Ingrams asked me to pull together a strategic plan for investing $56 million into the Cancer Center. I was shocked. Well it’s even better than that because they called me a few days later and said come up with a phase two plan to use $60 million more.
Ingram: He came back a couple months later with an answer. It was a 10-year strategic plan with two different five-year components. I said, “Is this designed to make the Cancer Center the best in the country?” and he said, “No, the best in the world.”
Moses: We got permission from the family to name the center for Bronson. The official name is E. Bronson Ingram Cancer Center at Vanderbilt but we talked with PR people and came up with Vanderbilt-Ingram Cancer Center with the agreement of the family.
Ingram: After that I was asked to head the Board of Overseers and volunteered to raise the balance to finish the strategic plan. The university was nervous to go public with the $150 million goal, so we set it at $100 million, but we blew through that quickly and announced the 150. As we neared the end we realized that research and technology were changing and increased the goal to $175 million and actually raised more beyond that.
Moses: That was money that we used to recruit a lot of people in conjunction and collaboration with departments. We set up some of the best shared resources in the country. I will admit I never wanted to be a cancer center director for the simple reason I didn’t want to do fundraising. I thought it was like begging. But I finally agreed to get into it and realized it’s not begging. It’s really interesting, very nice people who have money they can give and want to do good things with it, and you can offer good things to do with their money. That was actually one of the things I enjoyed most in my 12 years.
Marnett: We didn’t get Comprehensive status on our first renewal but came very close.
Moses: To be Comprehensive you had to have the basic, clinical, and prevention and control research and they had to talk to each other. We didn’t have the third prevention component. So we pulled together what we thought was good prevention and resubmitted in October 1998. We did well in our review and were site visited in January 1999 and received a 151 score. Big improvement. But they did not give us Comprehensive designation because they said our prevention was not what they wanted. We needed something like stop smoking campaigns or get your colonoscopies or population-based research. By that time we had brought Ray DuBois in as our prevention and control associate director. So Ray and I tried to recruit some epidemiologists.

1. Former Vanderbilt Chancellor Joe B. Wyatt with Martha Ingram at a 1999 reception to honor the late E. Bronson Ingram and kick off the “Imagine a World Without Cancer” $100 million fundraising campaign. 2. Members of country music group Blackhawk, longtime VICC supporters, visit with Hal Moses, M.D., and Frances Williams Preston in 1996.
DuBois: It’s very difficult to recruit epidemiologists because their cohorts are usually located at their home institution and often not moveable. But Bill Blot was running a consulting team and thought some of his folks might want to move to Nashville. That really catalyzed the whole epidemiology effort, especially the Southern Community Cohort Study.
Moses: At this point we could make an interim request for Comprehensive status. By that time I was not only on the committee that reviewed cancer centers, I was chairing it. I had to go back to my hotel room while they deliberated. They were absolutely forbidden to talk to me, but I had convinced one person, and I won’t give a name, who owed me a little bit to let me know it passed.
DuBois: Comprehensive status is something everyone strives for. We had gone from zero to something pretty significant in a short period of time.
In 2005, Moses resigned his leadership role to become director emeritus and DuBois was named director. After two years, he accepted a position at MD Anderson Cancer Center, and Pietenpol served as interim director while a national search was conducted. She was named director in 2008.
Beauchamp: Hal is a very good leader, I would say visionary. It’s not easy to put together all these different pieces and have them function in a coordinated way, and he was able to do that. He was very well organized and knew how to get people motivated.
Ingram: He’s a great visionary but is also good at implementing that vision. Those two things don’t always go together, but Hal has the rare ability to be a visionary but also an implementer.
Moses: I first met Jennifer Pietenpol after her first year of college. She went to Carleton College and was a classmate of my younger daughter. Jill’s birthday is July 3 and my wife had a party for her and invited her high school friends and all of the local Carleton students. So Jennifer came to the party and was pressuring me to get her a summer job at the Mayo Clinic. Her job that summer was a checker at a grocery store.
Pietenpol: I think it was fall/winter of my sophomore year of college I got a call from Hal and he said, “I couldn’t arrange for you to work in my lab because I have a returning college student for the coming summer, but I have found you a position in cardiology,” which I accepted. The following summer I worked in Hal’s lab and as irony would have it he took a position as chair of Cell Biology at Vanderbilt. It was shortly after Hal discovered the growth inhibitory properties of TGF-beta, very exciting times.
Moses: I talked her into coming to graduate school here in 1986. She was fabulous. She left to do postdoctoral training at Johns Hopkins and then she was one of the first people we recruited when we were building up the cancer research here in 1994.
Pietenpol: I was applying to graduate schools and asked Hal to write letters and I can remember him saying, “Well if I’m going to write letters for these other programs, why won’t you apply to Vanderbilt?” I had many decisions to make, but I can always remember being really influenced by observing that Hal was someone who really cared about the people who worked with him, and he really had the best interest of people at heart.
Moses: My recruiting philosophy is to try to get people better than I am. That raises me up. I’m not intimidated by many people. When I was thinking about stepping down as director, I really wanted someone to come in who had been better than I had been. She has been.
Pietenpol: [Vice Chancellor for Health Affairs] Harry Jacobson asked if I would be interim director. I didn’t have a dog in the hunt. It was not a position I was interested in, but I was incredibly loyal to the Cancer Center and to Vanderbilt. I said to Harry, “Absolutely, I will take care of the Cancer Center until you find a director because it is near and dear to my heart.”
Day: Jennifer Pietenpol is a great leader. She seemed like she came out of nowhere. She does leadership so well but is also a top-notch basic scientist. I’m a huge fan of hers.
Mills: She’s still just as full of energy and devotion and brilliance today. Then she was just younger and wore her hair in a ponytail.
THE HEART
Beauchamp: The greatest accomplishment is the collection of really talented people we have. That’s what I think we can be the most proud of at the Cancer Center. It’s not buildings. It’s people and what we can actually do for patients.
DuBois: The Cancer Center established a group of scientists working as a team. Before it was individual investigators on individual grants. Different components began working together as a team and that elevated the overall quality of care. It led to extending and saving lives that may not have happened before being put under one roof.
Day: The organization seen in cancer centers doesn’t exist in other major diseases like cardiology or mental health. We’re fortunate to have them because people can go to any of these centers around the country and get state-of-the-art care. If not for Vanderbilt, a cancer center wouldn’t have happened in Nashville.
Johnson: I think the clinicians, nurses and support staff who provide the great care deserve recognition. Ultimately what makes VICC so great, in my opinion, is that it delivers on what it promises—the right treatment given to the right patient at the right time by compassionate caregivers. It may start in the lab, but it ends at the patient. A cancer center that doesn’t deliver the best possible care is like Niagara Falls without water—not all that awe inspiring and pretty meaningless.
Beauchamp: We have over the 20 years experienced tremendous growth of our clinical cancer services and numbers of patients we serve. We are and have been for about a decade the top preference for patients in this region for cancer care.

Jennifer Pietenpol, Ph.D., at work in her lab in 1997.
Pietenpol: I never would have predicted 20 years ago that we would be doing what we’re doing now, particularly in terms of personalized medicine and tailoring treatment to a patient’s specific genes. We just didn’t have the technologies or the wherewithal to be where we are today.
Mills: I like to say we’re not a little mom and pop cancer center anymore.
Ingram: Vanderbilt has a great product to offer. It treats patients with respect and gives them hope when they may not get it anywhere else.
Moses: Cancer is far more complex than we could have imagined 20 years ago. It’s not just a hundred diseases, it’s thousands.
Beauchamp: I think what we’re going to see over the next 20 years is not a single cure for cancer because cancer is too many diseases. What we are going to see is chipping away, the 5 or 10 percent at a time based on the discoveries understanding the pathways that are driving cancer.
Ingram: I hope they’re all put out of business. In the best of all worlds, it would be great if they all had to learn a new profession. Realistically, I hope we can identify the disease earlier and have more person-specific treatment, to identify the problem and be able to fix it. Then they can all go fishing.
Johnson: For anyone who has had the opportunity to be part of building a highly successful program, there is nothing more gratifying.
Pietenpol: It’s a huge privilege. It’s two decades of work of a lot of people. I love one of the quotes of B.F. Byrd [former Vanderbilt clinical professor of Surgery and founding member of the VICC board of overseers]. He said, and I won’t get it exactly right, “My attitude is that you have to be involved. Some things take time, some things take money, some things take concern—you do each of the things when you need to.”
I think that’s what this 20 years is. Everyone in this community gave what they were good at giving at the time it was needed. It’s not one person or one moment in time or one gift, it’s actually a culmination, and it is still the case today. That is why we have this phenomenal Cancer Center, and it truly is a collective celebration.
