Weighing the Odds
Is Obesity Tipping the Scales Toward Cancer?
March 21, 2012 | Carole Bartoo
 Timothy Zeien had quite a list of concerns surrounding his weight – but cancer was not among them. At 230 pounds, the 64-year-old had type 2 diabetes and was taking cholesterol- and blood pressure-lowering medications.
Timothy Zeien had quite a list of concerns surrounding his weight – but cancer was not among them. At 230 pounds, the 64-year-old had type 2 diabetes and was taking cholesterol- and blood pressure-lowering medications.
In February 2011, Zeien made a major decision: to undergo a bariatric procedure called gastric sleeving. He says doctors had been encouraging him to do something for a long time, but he became serious about it when he and his wife moved to Tennessee to help their daughter, a pediatric emergency physician at Vanderbilt, with her children.
I was huffing and puffing up all these hills around here, and I thought ‘I don’t want to be a burden on my wife or children,’” Zeien said. “I’d like to see my grandchildren grow up, and I want to be a help.”
While cancer may not have been on Zeien’s list of concerns, experts say it should have been.
Weighing the odds
This decade, several large studies have made it clear that obesity and being overweight increase the rates of several cancers. The current estimate from leading cancer research groups is that 110,000 cancer deaths in the United States every year can be attributed to obesity, making it the second leading cause of cancer deaths, behind smoking.
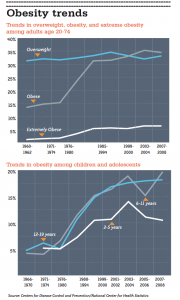
More than half of all American adults are overweight or obese – and that number continues to rise.
While many of the health risks associated with obesity – including heart disease, type 2 diabetes, and stroke – are widely recognized, the link between obesity and cancer has largely escaped notice. Surveys show people still believe little is known about what causes or could prevent cancer, and they do not associate cancer with obesity.

Like many people, cancer survivor Timothy Zeien did not associate obesity with increased cancer risk – even though he had a type of cancer linked to obesity. (Photo by Joe Howell)
“It’s true the mechanism may be murky,” admits Roger Cone, Ph.D., Joe C. Davis Professor of Biomedical Science, director of the Vanderbilt Institute for Obesity and Metabolism and chair of the Department of Molecular Physiology & Biophysics. “But the epidemiology is pretty straightforward. Meta-analysis shows that obesity may account for 14 percent of total deaths from cancer, and 20 percent of cancer deaths in women.”
Zeien says he had heard some of the news linking cancers to obesity. He even had one of the cancers listed among those most strongly linked to obesity: a kidney cancer removed about 15 years ago. But the idea that his own cancer might have been linked with his weight had never occurred to him.
“I don’t know why I ended up with cancer, but probably because of pesticide exposure, stuff around the house that is off the market now,” Zeien said.
An annual survey from the American Institute for Cancer Research (AICR) finds Zeien is in good company with that belief. In a 2010 survey, 71 percent of Americans said they believe cancer is linked with pesticides. Fifty-eight percent list food additives and 49 percent cite hormones in beef as causes of cancer. This despite an AICR Expert Panel review of the current literature which finds little evidence to link any of these potential risks with rates of cancer.
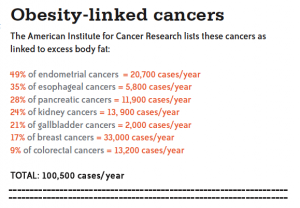
In stark contrast, the AICR report links seven cancers as “strongly associated” with obesity: endometrial, esophageal, pancreatic, kidney, gallbladder, breast (in post-menopausal women) and colorectal cancers.
While cancer tops the list of public health concerns year after year, and obesity has risen to the second leading concern, a disconnect remains. Nearly half of our population reports the two are not linked, and just as many believe it is impossible to prevent cancer.
If the case against smoking is any example, strong scientific evidence linking lifestyle habits to cancer can take a very long time to effect change. Gallup polls suggest the rate of smoking in the U.S. is just now approaching half the rate it was in the 1940s. After several decades of debate and increasing public prevention programs – even citywide bans on smoking – deaths from lung cancers are finally on the decline.
Smoking continues to be the No. 1 cause of cancer deaths through lung cancer, which currently accounts for nearly 30percent of all cancer deaths. But consider this: if lung cancer is removed from the equation, smoking is only linked with 12 percent of cancer deaths in men and 6 percent in women.
According to the AICR figures, obesity’s impact may exceed those rates, causing 14 percent of all cancer deaths – and 20 percent of cancer deaths in women.
Evidence of obesity’s link with cancer is not difficult to find. A well-publicized New England Journal of Medicine (NEJM) study of 900,000 adults in 2003 found the rate of death from many cancers (including leukemia and multiple myeloma) increased with a person’s degree of obesity. The heaviest people (those with a body mass index, or BMI, of at least 40) had cancer death rates 52 percent higher for men and 62 percent higher for women.
Obesity’s “deadliness factor” can seem small compared to other types of cancer risk factors. For example, hepatitis C increases risk of liver cancer by 1,600 percent; in contrast, obesity only confers a 100 percent increased risk of liver cancer.
However, the scale of obesity’s impact may be much broader since it affects so many people: only about 1.5 percent of Americans have a chronic hepatitis C virus infection, while 30 percent are obese.
The big “why?”
Part of obesity’s role in cancer is likely to be causative, and part of it is in its power to make outcomes worse. How much is one or the other is not known, but scientists at Vanderbilt say there is no longer any question that cancer is a worrisome part of our obesity epidemic.
Sorting out the hows and whys is now a hot topic in cancer research at Vanderbilt and around the world. But word has not yet reached street-level.
“The big question is how does obesity go about increasing cancer risk? The answer is still out and there could be multiple factors,” said William Blot, Ph.D., professor of Medicine and associate director of Cancer Prevention, Control and Population-based Research. “As we gain more information, we might be better able to develop strategies to prevent obesity-related cancer.”
Blot and other Vanderbilt colleagues are laying the epidemiologic groundwork to provide evidence in greater detail. Some of the most recent population-based findings highlight the complexity.
Blot is studying populations in the U.S., comparing the impact of obesity on death rates in people of different ethnic backgrounds. The Southern Community Cohort Study tracks a group of 86,000 adults throughout the South where obesity is prevalent. About two-thirds of this population is African-American and one- third is Caucasian.
“All causes of death in this cohort, including cancers, appear less striking among blacks. Our initial observations are that obesity may not convey the same risk as it does with whites. What seems to be emerging is a BMI around 30 (the standard for obesity) is not associated with increased risk of death in African-Americans. Whereas a BMI of around 25 seems optimal among whites, there may be a different pattern for blacks that requires further evaluation,” Blot says.
These findings apply to all causes of death, including the obesity biggies: diabetes and heart disease. But digging down further, Blot says cancer may be different in one respect. Ongoing research suggests being overweight as a youth may diminish these racial disparities in cancer risk – but not for the better.
“When we look at BMI at age 21 as a predictor of cancer risk later in life, at 40 or 60, we see almost the same pattern in blacks and whites, with increased risk among those who were obese in early adulthood. But we’re continuing to look at those numbers,” Blot said.

Wei Zheng, M.D., Ph.D., MPH, and colleagues have found that the health effects of obesity vary among different populations. (Photo by Daniel Dubois)
Wei Zheng, M.D., Ph.D, MPH, Ingram Professor of Cancer Research, chief of the Division of Epidemiology and director of the Vanderbilt Epidemiology Center is lead author of an August 2011 NEJM article that looked at more than 1 million people in China, Korea, Japan, India and Bangladesh. The picture of obesity and its impact on death from many causes including cancer was similar to what is seen in the U.S. and Europe, with one surprising exception.
“We were a little surprised that south Asians (those in Indian and Bangladesh) had no increased risk of death associated with overweight or even obesity,” Zheng said.
Rather than suggesting some populations may not be at risk from obesity, Zheng explains that large studies that go on for a long time – like his, which goes back 20 years – can be impacted by many factors, including poverty, famine and political strife. Zheng says his research illustrates that the picture of obesity is in flux around the world, making it difficult for public health officials to zero in on a message that applies to everyone. Nevertheless, looking into the future, prevention of obesity should be considered a priority even in less developed countries where obesity has gradually become an important public health problem over the past 10 years.
Biology of obesity
As Zheng and Blot work out the statistics in their population-based research, basic scientists like Cone work to describe what’s happening beneath skin level.
“We study rare syndromic obesity in order to find the genes and pathways involved in obesity,” Cone said.
Cone says there are several theories about why obesity may lead to cancer, including chronic inflammation or hormone imbalances, among other things. But the answers will likely include a combination of factors that differ for every cancer. Meanwhile, there are plenty of red flags to investigate. One of Cone’s mouse models helped describe leptin’s role in appetite and obesity. Now leptin is among a myriad of biochemicals being examined for their connection to obesity-related cancers. A partial list of work in the past decade includes:
• A Norwegian study found a threefold increase in the risk of colon cancer for those people who had the highest levels of leptin in their blood.
• Strong evidence from several studies suggests that endometrial cancers can occur because insulin resistance (common in obesity) leads to chronic progesterone deficiency.
• Several studies indicate that chronic high levels of insulin in the blood from insulin resistance also increase the risk of cancers of the colon and probably of the pancreas and kidney.
• New Vanderbilt research links an increase in deaths from glioma brain tumors to high levels of insulin in patients who are obese and have diabetes.
• Several studies show serum levels of insulin-like growth factor 1 (IGF1), increased in obese people, are associated with different forms of cancer.
• The hormone adiponectin stems the growth of cells and may prevent proliferation or cancer spread, but its levels decline with being overweight. Low levels are associated with breast cancer risk.
But for now, even Cone says the most intriguing evidence is coming from population-based studies. A 2009 NEJM study found women who had bariatric surgery reduced their cancer risk by 40 percent, although men who had the surgery had no such reduction in cancer risk.
The bariatric studies are still small, and even Zeien’s bariatric surgeon, Ronald H. Clements, M.D., director of Vanderbilt’s Center for Surgical Weight Loss, says it doesn’t suggest a clear public message at this time. Clements gave the talk that Timothy Zeien went to last year.

Ronald Clements, M.D., helps patients tackle obesity with bariatric surgery. (Photo by Daniel Dubois)
Clements says his talks include cancer among the devastating diseases obesity causes, and he mentions early evidence suggesting that bariatric surgery (and the resulting weight loss) may reduce cancer risk along with risk for diabetes and heart disease. But he is not at all certain that this knowledge and public health messaging about obesity will be an effective prevention.
“Unlike smoking, you need to eat to live,” points out Clements. “People who come to me have tried for years to lose weight without success. These are well-adjusted people, many of them with great jobs and full lives, so why is one person morbidly obese and their colleague is not? There is a genetic component, but we don’t fully understand it.”
Cone’s research seems to back this up, suggesting that at least a small number of people do indeed have a very difficult set of genes to overcome. But Cone has a different view, saying stronger public programs to prevent obesity early on, especially in childhood, could help the majority of people. In fact, he says prevention may be the only viable hope for most of our future population.
“If you are obese by age 15, you have an 80 percent chance of obesity as an adult,” Cone said.
Roger Cone, Ph.D., is probing the basic biology of obesity. (Photo by John Russell)
None of the researchers interviewed for this article felt strongly that anti-obesity messages would benefit from adding a line about cancer risk, or that the evidence is clear enough to determine what to say about cancer risk at this point. But Blot says a good sign is that much of cancer research funding from the National Institutes of Health (NIH) is now obesity-related. In fact, obesity’s contribution to cancer is one of the National Cancer Institute’s set of 24 “Provocative Questions,” an initiative to influence and guide cancer research funded by the institute by addressing important scientific questions that could drive progress against cancer.
If Blot’s own research bears out the theory that obesity early in life is a predictor of cancer risk that crosses lines of socio-economics and ethnicity, perhaps messaging will become more urgent. Perhaps a fire will be lit under public campaigns such as the FDA’s recently stalled effort to develop voluntary regulations on junk food advertisers who target children.
Whatever form the message takes or source it comes from, it is likely to take many more deaths from cancer and other obesity-related diseases before the public gets the message.
Zeien, who is 60 pounds lighter six months after he spent tens of thousands of dollars on his own bariatric surgery, is among the millions of people scientists will continue to watch and study. But his concerns about obesity aren’t so much about evidence and public health messages. They fall much closer to home.
He says his son, a hard-working father and physician in Florida, is also overweight. Like so many Americans, his son is well aware obesity poses risks, whether cancer is on his list of risks or not. The trouble is that the potential health consequences of obesity lie somewhere off in the future. Zeien hopes to encourage his loved ones by example, but says people have to come to the same sort of personal revelation he finally came to a year ago.
“It’s like a burglar alarm. Why do people buy burglar alarms after they have a break-in when they know about prevention? For me (weight loss) became important enough for my well-being, and maintaining my ability to help the family. That finally made it worth it.”
To learn more, see the National Cancer Institute’s list of “Provocative Questions” at provocativequestions.nci.nih.gov/rfa
(Scale photo by Lauren Owens)
Categories: Featured Story • Spring 2012
Tags: bariatric surgery • cancer • cancer prevention • cancer risk • epidemiology • NCI • obesity • Provocative Questions • Roger Cone • Ronald Clements • Wei Zheng • William Blot
Previous Post: Shape the Future
Next Post: News From Around the Cancer Center