Understanding Stem Cell Transplant
June 29, 2012

Vanderbilt-Ingram Cancer Center performs around 215 stem cell and bone marrow transplants each year, providing care leading up to the transplant, through all aspects of the procedure, and indefinitely after the transplant to monitor for complications. To address some common questions about the procedure, we spoke with Madan Jagasia, M.D., director of the Outpatient Transplant Program and section chief for Hematology and Stem Cell Transplant at Vanderbilt-Ingram.
What exactly are “stem cells” and where do they come from?
Stem cells – or more specifically, in this case, hematopoietic stem cells – are cells that can give rise to all the different types of mature blood cells – the red blood cells that carry oxygen, the platelets involved in blood clotting, and a host of white blood cells, which are part of the body’s immune system and provide defense against infectious agents. Stem cells are self-renewing (i.e., they can produce more of themselves) and reside primarily in the bone marrow but also circulate in the blood.
For a stem cell transplant, the stem cells can come from a related or unrelated donor, from umbilical cord blood, or from the patient him/herself.
Are these stem cells related to “embryonic stem cells?”
No, these are adult stem cells, from the blood or bone marrow. Even when the source of stem cells is umbilical cord blood, these are still adult stem cells and have nothing to do with embryonic stem cells.
What is the purpose of a stem cell transplant?
Most of the stem cell transplants we do in adult patients are for bone marrow, blood or lymph node cancers. For example, in acute leukemia, the DNA of immature white blood cells is somehow damaged, which causes one or more of the white blood cell types to grow rapidly and accumulate in the blood. These abnormal cells do not function properly and crowd out normally functioning blood cells.
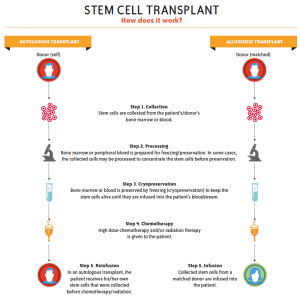
With a stem cell transplant (SCT), the patient’s stem cells are replaced with stem cells from either a healthy donor (called an “allogeneic” transplant) or with the patient’s own stem cells (called an “autologous” transplant). The goal is for the new stem cells to begin producing a new, properly functioning set of circulating blood cells.
Transplants can also be used to treat other blood and bone marrow diseases, like sickle cell anemia or thalassemia, for example.
Why would you put a patient’s stem cells back into them? Wouldn’t that cause the disease to come back?
An autologous transplant is more like a stem cell “rescue” than a true transplant – it is just removing the stem cells and giving them back to the patient. We do bone marrow biopsies as part of the transplant process to make sure that the marrow is not heavily contaminated (with malignant cells). And from previous research, we know that if/when the cancer comes back, it is because of residual cancer cells in the patient that were not killed by the chemotherapy, not from the stem cells that were infused back.
What is the transplant process like? (See graphic at right)
In an autologous transplant, we collect the patient’s stem cells, treat the patient with high-dose chemotherapy and/or radiation to hopefully kill the cancer and destroy the existing bone marrow, and then infuse the stem cells back intravenously, which become the new marrow.
In donor (allogeneic) transplants, we don’t always need as high a dose of chemotherapy for adult patients. The goal of the chemotherapy (in some patients, radiation is used along with chemotherapy) is to kill the recipient’s immune system, so that the donor cells won’t be rejected. The donor immune system then fights the tumor – a phenomenon that is called graft-versus-tumor effect.
What happens to the stem cells after they’ve been infused?
The infused stem cells find their way to the bone marrow, where they will start producing blood cells. This generally takes around two weeks, but can take longer (three to four weeks) for stem cells from umbilical cord. By monitoring blood cell counts, we know when this “engraftment” of the stem cells has occurred.
In time, the donor cells – which we call the “graft” – begin attacking the patient’s remaining tumor cells. We call this “graft-versus-tumor” effect, and that’s what leads to remission or cure.
If the “graft” is attacking my tumor, will it also attack the rest of my healthy tissues?
Possibly. The challenge in allogeneic transplants is something called “graft-versus-host disease” (GVHD). The graft doesn’t really know the difference between a patient’s tumor cells and healthy cells, so the donor cells may attack healthy tissue. GVHD is the bottleneck of transplantation today, so we try to limit or treat the damage done by the donor’s immune cells with steroids and other therapies. (See “When the Treatment Fights Back“)
What is the chance a stem cell transplant will “cure” the cancer?
The “success rate” or “cure rate” – the percentage of patients living five years or more beyond transplant – just depends on the disease for which the transplant was done and the source of the cells transplanted. To give examples of the extremes: for a person in their 20s with aplastic anemia (a bone marrow failure syndrome) receiving a related donor transplant, the cure rate is about 90 percent; on the other extreme, for someone with advanced relapsed leukemia receiving stem cells from umbilical cord blood, the cure rate might be between 10 percent and 15 percent.